
 Rapa FM Pader
Rapa FM Pader

 Rapa FM Pader
Rapa FM Pader
16 November 2024, 08:32

By Lakomekec Kinyera
A concerning new study from Uganda has revealed the emergence of partial resistance to artemisinin—the most effective malaria drug—among African children with severe malaria. This discovery, presented at the Annual Meeting of the American Society of Tropical Medicine and Hygiene and published in The Journal of the American Medical Association (JAMA), raises serious concerns about the future of malaria treatment, particularly in sub-Saharan Africa, where the disease remains a leading cause of death.
The study, conducted on 100 children aged six months to 12 years with severe malaria caused by Plasmodium falciparum, identified signs of partial resistance to artemisinin in 11 children. Ten of these children experienced malaria relapses within 28 days, infected by the same strain that caused their initial illness. This represents the first documented case of artemisinin resistance in Africa, raising alarms about the future efficacy of artemisinin-based combination therapies (ACTs), which have been central to the fight against malaria for over two decades.
The research also identified genetic mutations in the malaria parasites of 10 children. These mutations, linked to artemisinin resistance, had previously only been observed in Southeast Asia, where resistance was first detected in 2008. This finding signals a pivotal moment for malaria treatment in Africa, where the disease burden remains exceptionally high.
This evidence of resistance emerges at a time when malaria remains a leading cause of death in sub-Saharan Africa, accounting for 95% of global malaria fatalities, with most victims being children under five. The spread of artemisinin resistance, which began in Southeast Asia and has now reached East Africa, including Uganda, threatens to reverse the progress achieved in reducing malaria-related illness and death.
Experts fear that the pattern observed in Southeast Asia—where delayed parasite clearance eventually led to complete drug failure—could be replicated in Africa. This underscores the urgent need for new malaria treatments, strengthened control programmes, and robust monitoring of drug efficacy.
Uganda remains at the epicentre of the malaria crisis, with the highest incidence rate globally—478 cases per 1,000 people annually. Malaria transmission occurs consistently throughout the year, peaking during the rainy seasons. Plasmodium falciparum accounts for 98% of cases, with P. vivax and P. ovale being rare.
Malaria continues to be a leading cause of illness and death in Uganda, responsible for up to 40% of outpatient visits, 25% of hospital admissions, and 14% of hospital deaths. Children are disproportionately affected, with 9% of those under five suffering from malaria, while pregnant women also face significant risks.
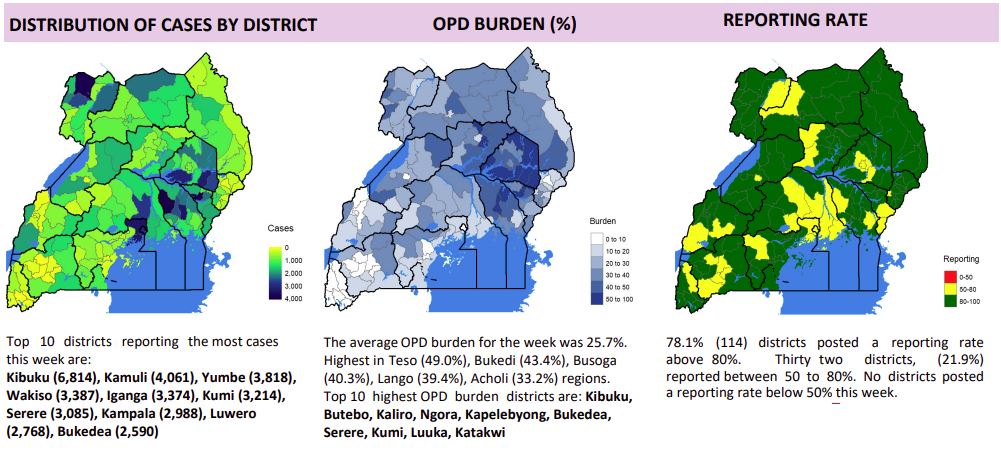
Recent data from February to March 2024 reveals a test positivity rate of 41.7%, with 166,772 confirmed malaria cases reported during this period.
Pader district, one of the most severely affected regions in Uganda, continues to grapple with a devastating malaria crisis. As of 11 August 2024, the health department reported 5,362 malaria cases across all health sectors, making Pader the district with the highest number of cases in the Acholi sub-region.
Malaria accounts for 61% of outpatient visits in Pader, highlighting the critical nature of the situation. Tragically, four children succumbed to malaria in the last quarter, underscoring the urgent need for strengthened interventions.

Mr. Sipriano Odong, the malaria focal person at Acholibur Health Centre III, has criticised the community for neglecting preventive measures, including self-medication and the improper use of mosquito nets. He highlighted that delayed reporting for treatment and a lack of commitment to prevention are significant factors contributing to the high mortality rates in the district.
“The community has been neglecting prevention efforts, particularly through self-medication and the misuse of mosquito nets. This has resulted in late reporting for treatment and a poor attitude towards prevention, which ultimately contributes to the high mortality rate,” said Mr. Odong.
He also stressed the importance of early treatment: “We must prioritise the proper use of preventive measures and ensure that people visit health centres as soon as they show signs of malaria. Timely treatment is essential to saving lives.”
The findings from this study, coupled with Uganda’s ongoing malaria crisis, underscore the urgent need for immediate intervention. Malaria not only imposes a substantial health burden but also presents significant social and economic challenges, particularly for the poorest and most vulnerable populations. Experts are urging accelerated efforts to develop new malaria treatments, enhance existing control programmes, and promote public awareness and adherence to prevention strategies.
Uganda’s National Malaria Control Programme aims to ensure equitable access to malaria services and improve health equity. However, meaningful progress will require intensified efforts from the government, local communities, and international organisations. Addressing the growing threat of artemisinin resistance and working towards the long-term elimination of malaria must become top priorities.
“If the emerging resistance to artemisinin is not swiftly tackled, the progress achieved in reducing malaria cases and deaths over the past two decades could be undone,” warned an expert in tropical medicine. “Coordinated and urgent action is critical to prevent the escalation of this public health crisis and to ensure future generations are not lost to a preventable disease.”