 Mama FM
Mama FM
 Mama FM
Mama FM
6 February 2026, 11:59 am
Byamukama Alozious
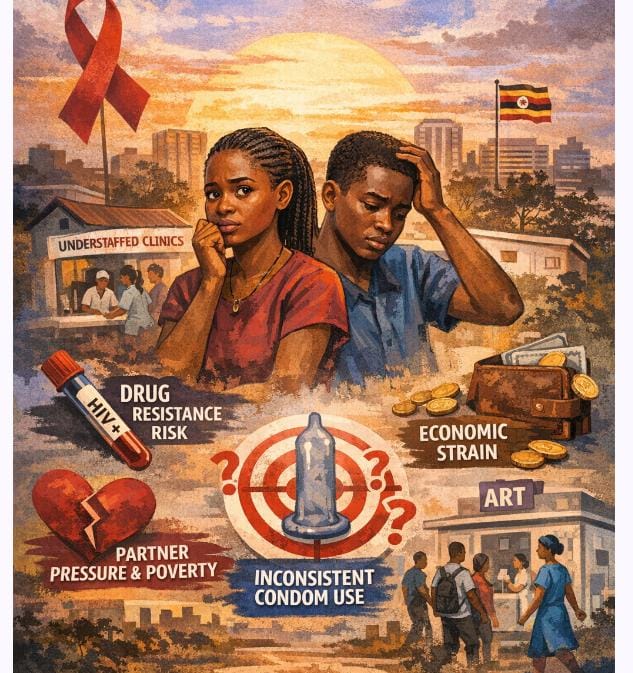
As Uganda moves deeper into 2026 HIV response, the country stands at a critical crossroads. New infections are increasingly concentrated among young people, funding for HIV programmes is tightening, and prevention efforts are under pressure to deliver results. In this context, evidence from a 2022 study on condom use among young people living with HIV in Central Uganda remains not only relevant, but urgent.
National Condom Day is commemorated annually in Uganda on February 13th, alongside the global International Condom Day, to promote safe sex, reduce HIV/STI transmission, and prevent unplanned pregnancies, often coinciding with Valentine’s Day
The study, Factors Associated with Condom Use Among Out-of-School Young People on Anti-Retroviral Therapy in Central Uganda, published in April 2022 in the journal HIV/AIDS – Research and Palliative Care (https://doi.org/10.2147/HIV.S357535), examined 357 out-of-school young people aged 15 to 24 who were living with HIV and already on antiretroviral therapy. Its findings reveal gaps that Uganda’s HIV response is still struggling to close in 2025—and risks carrying into 2026 if left unaddressed.
Nearly half of the young people studied, about 49 percent, reported inconsistent condom use. This is not an outdated statistic. It mirrors current national concerns about continued HIV transmission among adolescents and young adults, even as treatment coverage improves. In 2025, Uganda’s HIV strategy strongly promotes viral suppression, but the study reminds policymakers that treatment alone does not stop transmission. Inconsistent condom use among people on ART increases the risk of HIV re-infection, drug resistance, and onward spread, undermining progress made through years of investment in treatment.
As Uganda aligns its HIV response to global targets beyond 2026, condoms remain one of the most cost-effective prevention tools available. The study reiterates that male and female condoms, when used correctly and consistently, can be up to 95 percent effective. In an era where donor funding is shrinking and programmes are being asked to “do more with less,” ignoring such a low-cost, high-impact intervention would be a strategic mistake.
The social drivers identified in the 2022 study are still shaping HIV risk today. Fear of losing a sexual partner, non-disclosure of HIV status, and poverty were major reasons young people avoided condoms. These challenges have not disappeared. If anything, economic pressures facing young people in 2026—especially unemployment and rising living costs—have intensified. Young women, who made up the majority of study participants, continue to face unequal power in relationships, limiting their ability to negotiate safer sex. Any HIV response looking toward 2026 must confront these realities rather than assume that awareness alone changes behaviour.
The study also offers lessons for health system strengthening, a key focus of Uganda’s current HIV programming. Young people who believed their health facilities had enough health workers were six times more likely to use condoms consistently. This finding directly speaks to ongoing concerns in 2026 about overstretched ART clinics and staff burnout. Investing in human resources for health is not just about service delivery; it is prevention.